Table of Contents
Uveal melanoma or ocular melanoma is a rare but serious form of eye cancer that originates in the uvea, the middle layer of the eye. This condition can have significant implications for vision and overall health, making awareness and early detection crucial. Although uncommon, its impact can be life-changing, underscoring the urgency for vigilance and timely intervention.
In this comprehensive guide, we will explore uveal melanoma symptoms, diagnosis, and treatment options for uveal melanoma, aiming to provide a thorough understanding of this condition and ways to manage it effectively.
Understanding Uveal Melanoma: The Basics
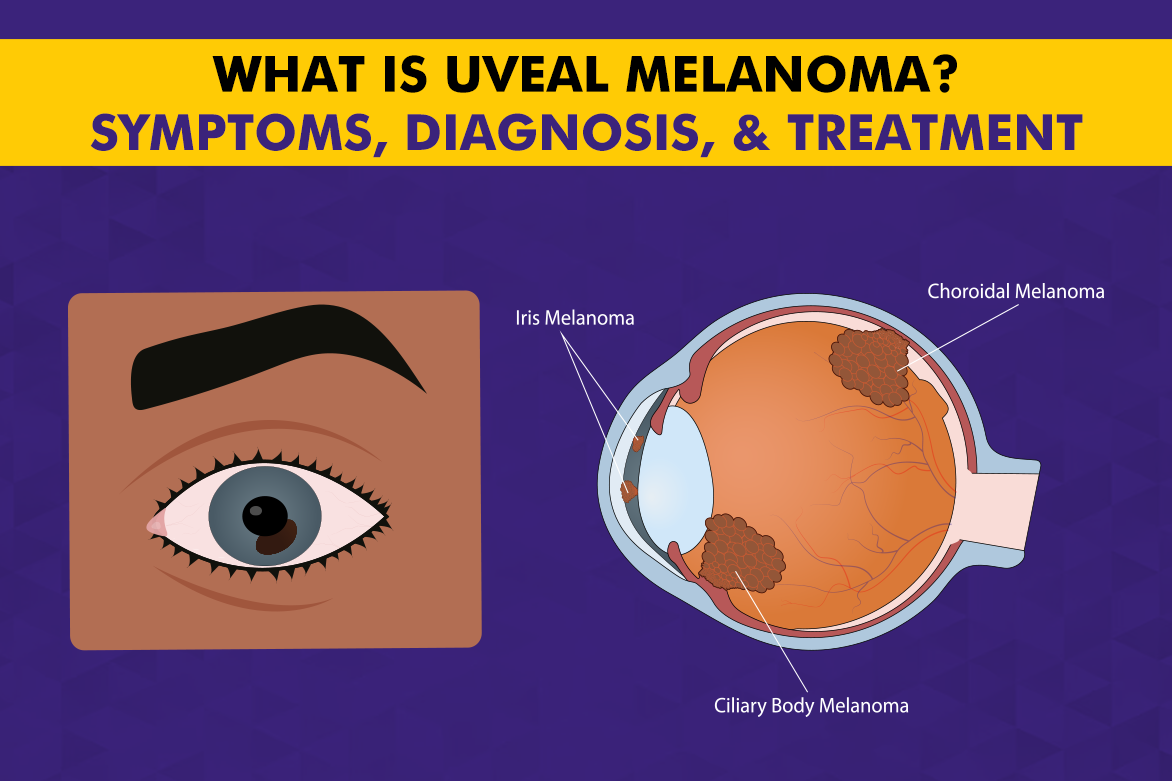
Melanoma in eye develops from melanocytes, the cells responsible for producing pigment in the eye. The uvea consists of three parts: the iris, the ciliary body, and the choroid. Melanoma can arise in any of these areas, but it is most commonly found in the choroid. Unlike its more familiar counterpart on the skin, uveal melanoma is hidden from plain sight, often progressing without obvious warning until it is advanced. Despite that this choroidal melanoma occurrence is rare, it is the most common primary intraocular malignancy in adults, affecting approximately 5 to 7 people per million each year worldwide.
Remarkably, this cancer can affect anyone, regardless of age or background, underscoring the importance of routine eye health checks, even for those who consider their vision perfect.
Recognizing the Symptoms: What to Watch For
Early-stage uveal melanoma symptoms are often difficult to detect, as they can be subtle or easily overlooked.
- One of the most common early signs is a gradual change in vision, such as persistent blurred vision or the sudden appearance of floaters, tiny spots or threads drifting across your field of sight.
- You might also notice a small, dark spot on the iris, or experience a reduction in peripheral (side) vision.
- Occasionally, the shape of the pupil can appear irregular or altered.
These changes are rarely painful and may seem insignificant; they are easily mistaken for minor or age-related eye issues.
Causes and Risk Factors
The underlying causes of choroidal melanoma are complex and not entirely understood, but research indicates that this cancer develops due to a combination of genetic, environmental, and biological factors that disrupt the normal function of melanocytes—the pigment-producing cells of the eye. Mutations in specific genes can trigger these cells to multiply uncontrollably, leading to eye cancer formation. Environmental exposures, especially ultraviolet (UV) light, are believed to damage cellular DNA over time, increasing the risk for individuals with certain susceptibilities.
Risk factors for Uveal Melanoma that may elevate the likelihood of developing uveal melanoma:
- Fair Skin and Light-Colored Eyes: People with lighter skin and eyes have less natural pigment (melanin), offering reduced protection against UV radiation. This may make melanocytes more vulnerable to mutations.
- Age: The risk increases with age, with most cases occurring in adults over 50.
- Genetic Mutations: Certain inherited genetic conditions and gene alterations can predispose individuals to uveal melanoma.
- Family History: A family history of eye cancer or other related cancers can indicate a greater inherited risk.
- Exposure to Ultraviolet (UV) Light: Prolonged exposure to sunlight or may increase the risk, though the eye’s anatomy offers some natural shielding compared to the skin.
- Pre-Existing Eye Conditions: Conditions such as ocular or oculodermal melanocytosis have been associated with a higher risk.
How Is Uveal Melanoma Diagnosed?
Diagnosing uveal melanoma is a comprehensive process of ocular oncology, developed to accurately detect and assess the tumor’s size, location, and characteristics. This begins with a detailed eye examination performed by an expert eye cancer surgeon, who carefully inspects the structures of the eye for any abnormalities through:
- Ophthalmoscopy: The doctor uses a special lens and light to look inside the eye and directly visualize any suspicious growths on the uvea.
- Ultrasound Imaging: A small probe sends sound waves into the eye, producing detailed images that help measure the tumor’s dimensions and detect its exact position. It’s a painless, non-invasive test.
- Fluorescein Angiography: A dye is injected into a vein in the arm, which then circulates to the eye. Special photographs are taken as the dye passes through the blood vessels in the retina and choroid, highlighting abnormal patterns suggestive of melanoma.
- Optical Coherence Tomography (OCT): This imaging test provides highly detailed cross-sectional images of the retina and underlying tissues, helping specialists differentiate melanoma from other eye lesions.
- Biopsy (in select cases): If there’s uncertainty after imaging, a tiny sample of tissue may be removed from the tumor using a fine needle and examined under a microscope for cancer cells. Biopsy is generally reserved for cases where imaging is inconclusive.
Uveal Melanoma Treatment Options
Treatment for uveal melanoma is personalized based on the tumor’s size, location, and the patient’s health, with each option offering distinct approaches and potential outcomes. At Centre For Sight, you get world-class and specialized treatment for ocular oncology, including melanoma in the eye, through:
1. Plaque Brachytherapy (Radiation Therapy):
This is the most widely used treatment for small- to medium-sized tumors. A small disc, or plaque, containing radioactive seeds is surgically placed on the outside of the eye, directly over the tumor. The plaque delivers a focused dose of radiation to shrink the tumor while minimizing damage to surrounding healthy tissue. The plaque remains in place for several days and is then removed during a separate procedure.
Effectiveness: Highly effective for local tumor control, allowing most patients to preserve their eye and some vision, though the risk of vision loss increases near the macula or optic nerve.
2. External Beam Radiation Therapy:
This approach uses directed beams of energy (such as proton or gamma rays) from outside the body to target the tumor. The patient undergoes a series of precisely planned treatment sessions over several days or weeks.
Effectiveness: Effective for tumors that are not suitable for plaque brachytherapy. There can be a greater risk of side effects on surrounding eye structures, sometimes affecting vision. It is used when plaque therapy is not feasible but may have broader side effects.
3. Laser Therapy (Transpupillary Thermotherapy – TTT):
A specialized laser is used to heat and destroy tumor cells. TTT is typically considered for small, well-defined tumors or as an adjunct to other treatments. It is performed in a clinic setting with minimal discomfort.
Effectiveness: Suitable for select small tumors, but less effective for larger or thicker growths. Frequently combined with radiation therapy.
4. Surgical Removal (Local Resection):
For accessible tumors, surgery may be performed to remove the melanoma while sparing the rest of the eye. This can be technically complex and is generally reserved for specific cases.
Effectiveness: Offers the chance for tumor removal with eye preservation but carries the risk of complications and vision loss.
5. Enucleation (Removal of the Eye):
When the tumor is large, causing pain, or has destroyed vision, the entire eye may be surgically removed to eliminate the cancer and prevent its spread. A custom ocular prosthesis is later provided for cosmetic appearance.
Effectiveness: Most definitive way to stop tumor growth within the eye and prevent metastasis, but results in permanent loss of vision in that eye. – It is the last resort when vision cannot be salvaged or cancer control is urgent.
The best approach is determined jointly by patient and specialist, based on individual tumor characteristics and patient needs.
Monitoring and Prognosis of Uveal Melanoma
Regular follow-up visits:
- Help monitor the eye for any signs of the tumor returning (recurrence) or spreading to other parts of the body (metastasis).
- Allow timely detection of complications or late effects from treatment.
Prognosis:
- Varies significantly depending on tumor size, location, and specific genetic markers present in the cells.
- Early-stage detection offers a more favorable chance for vision preservation and long-term survival, reinforcing the value of early intervention.
Conclusion
Uveal melanoma is a serious condition that requires prompt attention and treatment. Understanding the symptoms, risk factors, and available treatment options can significantly improve outcomes for those affected.
Regular eye exams and awareness of changes in vision are key to early detection and successful management of this condition.